- Knee Anatomy
- Knee Pain Causes
- Knee Pain Treatments
- Stretching & Exercises
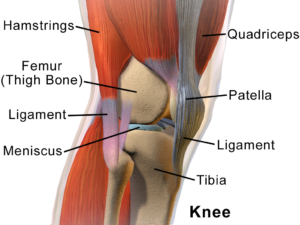 The knee is a “hinge” joint. The thigh bone (femur) is connected to the shin bone (tibia) by a series of muscles, ligaments (connecting bone to bone), and tendons (connecting muscles to bone). The knee cap (patella) overlies the knee joint providing added protection and stability.
The knee is a “hinge” joint. The thigh bone (femur) is connected to the shin bone (tibia) by a series of muscles, ligaments (connecting bone to bone), and tendons (connecting muscles to bone). The knee cap (patella) overlies the knee joint providing added protection and stability.
There are many ligaments that help stabilize the knee. The medial collateral ligament (MCL) lies on the inner aspect (medial) of the knee joint and protects it against excess inwards (valgus) force while the lateral collateral ligament lies on the outside (lateral) of the knee joint and protects it against excess outwards (varus) force. The Anterior Cruciate Ligament (ACL) and Posterior Cruciate Ligament (PCL) lie deep within the knee joint between the femur and tibia, preventing excess sliding movements of the knee joint.
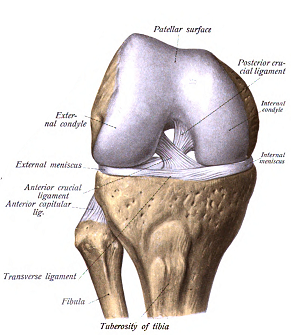 The knee cap (patella) is a circular bone that lies on the front of the knee joint. It is connected to the thigh (quadriceps) muscles by the quadriceps tendon and the shin bone (tibia) by the patellar tendon. It sits on top of the trochlear groove of the femur.
The knee cap (patella) is a circular bone that lies on the front of the knee joint. It is connected to the thigh (quadriceps) muscles by the quadriceps tendon and the shin bone (tibia) by the patellar tendon. It sits on top of the trochlear groove of the femur.
Inside the knee joint, on the upper surface of the shin bone (tibia) lies the medial and lateral menisci. A meniscus is a smooth C-shaped ring of cartilage that protects the knee bones from grinding against each other, and offers shock absorption to the knee joint. The knee joint also contains synovial fluid, which acts as a lubricant inside the joint.
There are many muscles that help the knee move. The quadriceps help the knee straighten (extension) and the hamstrings help the knee bend (flexion).
Knee Pain Causes
Knee Osteoarthritis
Osteoarthritis is the most common type of arthritis and the most common joints being affected include the knees, hands, hips and back. Some risk factors for osteoarthritis include age, obesity, past knee injury, occupational history and genetics. Over time, there is a breakdown of cartilage, triggering an inflammatory response. Affected joints have loss of cartilage, decreased joint space and development of bony spurring. Symptoms include joint pain that is worsened with movement and relieved by rest as well as morning stiffness. The pain is often described as a dull ache.
Diagnosis of knee osteoarthritis usually involves taking a complete history with regards to the knee pain, performing a physical exam and interpreting X-Ray findings.
Osteoarthritis is essentially irreversible in terms of the changes in the joint, however there are treatments to help manage the condition.
Patellofemoral Pain Syndrome (PFPS)
Patellofemoral Pain Syndrome (PFPS) is a common knee condition that is more common in younger adults but can affect anyone of any age. The main symptom of this condition is pain in the front of the knee or pain behind the knee cap (patella). Patients can sometimes have significant difficulty with activities of daily living due to the stiffness and pain that result. It is usually made worse by activities such as running, standing from a chair, prolonged sitting (also called the “theater sign”), or going up and down stairs. There may also be a sensation of “giving away” (instability).
This condition may develop when the knee cap (patella) moves incorrectly in its groove in the thigh bone (femoral trochlea), or there is too much loading stress on the patellofemoral joint during weight bearing on a flexed knee. Risk factors include overactivity, age (adolescence & second/third decade of life), and female sex.
PFPS is diagnosed based on clinical presentation, so there are no tests to confirm diagnosis, unless your doctor feels they need to rule out other conditions. In that case, your doctor may order X-rays or other imaging.
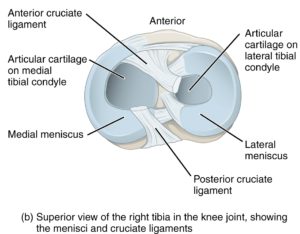
Meniscal Tears
Your meniscus is a C-shaped fibroelastic cartilage that acts as a shock absorber and also helps stabilize the knee. There are two of them, one on the medial (inside) and lateral (outside) aspect of the knee. In younger patients, these menisci can be injured in traumatic events and can become torn. Patients may recall hearing or feeling a popping or tearing sensation. In these cases, the knee may become swollen in the following hours after injury. There may be other associated symptoms such as instability, clicking, or locking, which when there is significant loss of passive range of motion, particularly extension. The pain is typically quite sharp and located on one aspect of the knee, and worse with pivoting/twisting motions and deep flexion of the knee.
In older adults, these menisci degenerate with time and can suffer from degenerative type tears. These are associated with osteoarthritis. These type of tears typically do not have a history of significant trauma. It can otherwise present in a similar fashion.
Meniscal tears are suspected based on the history and physical exam, and can be confirmed with imaging such as an MRI. An XRay does not show the meniscus but can provide other important information for your doctor.
Knee Pain Treatments
Knee Osteoarthritis:
Some non-medical treatment options include:
- Exercises – This has some of the best evidence to help maintain range of motion and strengthen muscles around affected joints. Specific programs such as the GLA:D program have had studies reporting significant improvement in patient symptoms and function.
- Activity modification (avoiding higher impact activities that trigger pain)
- Weight loss to help slow progression
- Knee braces to help with knee mechanics (ranging from sleeves to medial off-loader braces)
- Supplements such as glucosamine and chondroitin have mixed scientific evidence but may be considered.
Some medical treatment options include:
- Pain medications, including Tylenol/Acetaminophen
- Non-steroidal anti-inflammatory medications (Advil/Ibuprofen, Aleve/Naproxen or topical formulations such as Diclofenac/Voltaren)
- Steroid injections into the joint
- Viscosupplementation (Hyaluronic Acid) injections into the joint
- Platelet Rich Plasma injections into the joint
- Operative treatment if the above fail (eg. Partial or total joint replacement)
Patellofemoral Pain Syndrome (PFPS):
Some non-medical treatment options include (adapted from the 2018 consensus statement for patellofemoral pain treatment).
- Exercises – This has the best evidence for improving pain and function in the short, medium, and long term. You should get exercises designed to help maintain range of motion, alter loading patterns, and strengthen muscles around affected joints. These exercises should focus on both the hip and the knee for best results. Benefits can be expected 6–12 weeks after starting physiotherapy.
- Orthotics – if there are underlying biomechanical abnormalities of the feet this can be helpful for reducing pain in the short term. Both “off the shelf” and custom orthotics appear helpful.
- Bracing and Taping – Latest research is uncertain on whether bracing or supportive taping to improve alignment of the knee is helpful.
- Acupuncture or dry needling – Latest research is uncertain on whether acupuncture or dry needling is helpful.
- Manual therapy – Latest research is uncertain whether manual soft tissue techniques (ischemic compression to trigger pains and other myofascial techniques) is helpful.
- Mobilisations of the knee, patellofemoral joint, or lumbar spine – Latest research currently does not recommend mobilisations of these joints due to lack of evidence for benefit.
- Electrophysical agents (ultrasound, phonophoresis, laser therapy) – Latest research currently does not recommend electrophysical agents due to lack of evidence for benefit.
- Other interventions may include heat and/or ice as needed, or weight loss to reduce load on the knee.
Some medical treatment options include:
- Pain medications, including Tylenol/Acetaminophen.
- Non-steroidal anti-inflammatory medications, including Advil/Ibuprofen and Aleve/Naproxen.
- Operative treatment if the above fail (eg. Arthroscopic surgery).
Meniscal Tears:
Some non-medical treatment options include:
- Exercises – This has some of the best evidence to help maintain range of motion and strengthen muscles around affected joints.
- Activity modification (avoiding higher impact exercises or pivoting movements that trigger pain)
- Weight loss to help reduce stress on the knee
Some medical treatment options include:
- Pain medications, including Tylenol/Acetaminophen
- Non-steroidal anti-inflammatory medications (Advil/Ibuprofen, Aleve/Naproxen or topical formulations such as Diclofenac/Voltaren)
- Injections: If there is some osteoarthritis, injections as described for osteoarthritis can be considered (steroid, viscosupplementation, PRP)
- Operative treatment if the above fail (eg. menisectomy, meniscal repair)
Knee Osteoarthritis and Patellofemoral Pain Syndrome Exercises:
Many of these exercises involve a resistance band. These are elastic bands of varying resistance to make the exercise more challenging. These can easily be purchased at many retailers.
| Name | Repetitions/Set | Description (Basic) | Progression | Modified (Easier) |
| Hip Flexion (theraband) | 2-4 sets of 8-15 repetitions on each leg. Exercises should be performed 4-6x/week. | Attach one end of theraband to secure place and the other end to your ankle. Holding on to a chair for support, slowly raise your leg forward until you feel significant resistance, then slowly bring it back down to the ground.
Be sure that your toes are pointing upwards and your knees are locked straight. Be sure your hips, knees, and ankles are all in a straight line. |
To make things more difficult, you can choose not to hold on to the chair for support.
You can add an ankle weight for further increased difficulty. |
Lying on your back, bend one knee to 90 degrees and keep the other one straight. Slowly raise your straightened leg about 10 inches off the floor, hold it there for a count of 5-10, then bring it back down to the table. |
| Hip Extension (theraband) | 2-4 sets of 8-15 repetitions on each leg. Exercises should be performed 4-6x/week. | Attach one end of theraband to secure place and the other end to your ankle. Holding on to a chair for support, slowly extend your leg backwards behind you to about 30 degrees, or until you feel resistance, then slowly bring it back down to the ground. Be sure that your toes are pointing upwards and your knees are locked straight. Be sure your hips, knees, and ankles are all in a straight line and you are not moving excessively through the low back. | To make things more difficult, you can choose not to hold on to the chair for support and then changing to therabands with increased resistance | |
| Hip Abduction (theraband) | 2-4 sets of 8-15 repetitions on each leg. Exercises should be performed 4-6x/week. | Attach one end of theraband to secure place and the other end to your ankle. Holding on to a chair for support, slowly move your leg away from your body to about 30 degrees, or until you feel resistance, then slowly bring it back down to the ground. Be sure that your toes are pointing upwards and your knees are locked straight. Be sure your hips, knees, and ankles are all in a straight line. | To make things more difficult, you can choose not to hold on to the chair for support.
You can add an ankle weight for increased difficulty. |
Lying on your side, bend the bottom leg to 90 degrees in front of your body. Keep the other one straight. Slowly raise your straightened leg about 10 inches off the floor, hold it there for a count of 5-10, then bring it back down to the table. |
| Hip Adduction (theraband) | 2-4 sets of 8-15 repetitions on each leg. Exercises should be performed 4-6x/week. | Attach one end of theraband to secure place and the other end to your ankle. Holding on to a chair for support, slowly move your leg across your body to about 20 degrees, or until you feel resistance, then slowly bring it back down to the ground.
Be sure that your toes are pointing upwards and your knees are locked straight. Be sure your hips, knees, and ankles are all in a straight line. |
To make things more difficult, you can choose not to hold on to the chair for support
You can add an ankle weight for increased difficulty. |
Lying on your side, bend the top leg to 90 degrees in front of your body and rest your foot in front of the other knee. Keep the bottom leg straight. Slowly raise your straightened leg about 10 inches off the floor, hold it there for a count of 5-10, then bring it back down to the table. |
| Squat | 2-4 sets of 8-15 repetitions. Exercises should be performed 4-6x/week. | Stand in front of a chair securely placed on the ground. Stand with your feet firmly planted shoulder width apart, with your feet facing very slightly outwards. Extend your arms outwards in front of your body for balance. Very slowly lower your body down, hinging at the hips and knees until you feel discomfort or lack of balance then return to your starting position. Your feet should remain planted, your knees should never extend in front of your toes or collapse inwards, and you should feel your buttocks being pushed back as far as you can. | To make things more difficult, remove the chair and go into a full low squat.
You can also hold weights (such as a dumbbell in a goblet position) for added difficulty. |
To make things easier, try slowly squatting and lowering yourself into a chair, without using your arms to support yourself. Hold your arms outwards in front of your body for balance. Make sure the chair is positioned well and will not move. |
| Hip Bridge | 5-10 repetitions of 5-10 second holds. Exercises should be performed 4-6x/week. | Lie on your back with your hips and knees bent to 90 degrees and both feet planted firmly on the ground. Slowly raise your buttocks off of the ground, trying to make a straight line from your knees to your shoulders. Hold this position for 5-10 seconds, then slowly come back down to starting position. Be sure that your knees, hips, and shoulders remain in a straight line. | For added difficulty, perform this exercise with one leg straightened in front of your body. You can also carry a weight at your hips. |
