- Ankle Anatomy
- Ankle Pain Causes
- Ankle Pain Treatments
- Stretching & Exercises
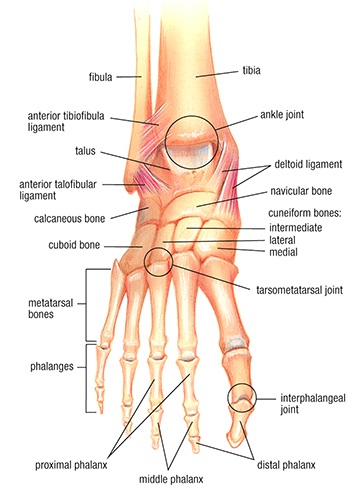 The ankle is a complex joint capable of movement in many directions. At the ankle, the bones of the lower leg meet the bones of the foot. The connection is solidified by a series of ligaments (connecting bone to bone) and tendons (connecting muscle to bone). The joint is called a synovial joint because the bones that move on one another are in a joint capsule and surrounded by synovial fluid. Cartilage helps provide a cushion where the bones meet.
The ankle is a complex joint capable of movement in many directions. At the ankle, the bones of the lower leg meet the bones of the foot. The connection is solidified by a series of ligaments (connecting bone to bone) and tendons (connecting muscle to bone). The joint is called a synovial joint because the bones that move on one another are in a joint capsule and surrounded by synovial fluid. Cartilage helps provide a cushion where the bones meet.
The motion of the ankle comes from two separate joints:
The main ankle joint is called the talocrural joint. This is the joint that allows up (dorsiflexion) and down (plantarflexion) motion of the foot. At this joint the fibula and tibia of the lower leg come together to create a pocket for the talus (bone) of the foot to sit securely. This pocket is called the mortise as it resembles a mortise and tenon joint in woodworking. The tibia and fibula are held together by connective tissue and various ligaments to form what is called the ankle syndesmosis.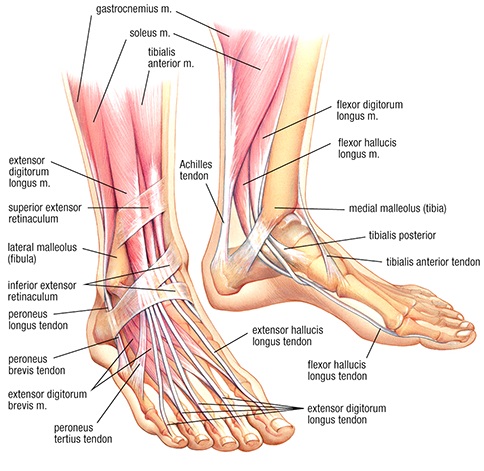
The outside (lateral) side of the main ankle joint is made out of 3 separate ligaments; the anterior talofibular, posterior talofibular and the calcaneofibular ligaments. The inside (medial) side of the ankle joint is made out of a group of ligaments together called the deltoid ligament. Plantarflexion is accomplished by the calf muscles pulling on the Achilles tendon while dorsiflexion is accomplished by muscles at the front of the shin.
Side motion of the foot/ankle occurs mainly at the subtalar joint. At this joint the talus (from the main ankle joint) meets the calcaneus (heel bone). This joint is held together by four main ligaments. Various muscles from the lower leg allow eversion (outward rolling of foot) and inversion (inward rolling of foot).
Achilles Tendinopathy
The Achilles tendon is located at the back of the foot and connects the calf muscles to the heel. Contraction of the calf muscles pulls on the Achilles tendon and allows you to go on your tip-toes (plantar flexion). Pain in the Achilles tendon is a common complaint and is often caused by Achilles tendinopathy. There are two main types of Achilles tendinopathy: insertional (where the tendon meets the bone) and non-insertional (at the middle of the tendon). Non-insertional is the most common type.
Achilles tendinopathy is thought to be an overload injury and commonly occurs in runners. It used to be thought that the injury was due to inflammation, but it now appears that the condition occurs because of abnormalities in the tendon. Symptoms of Achilles tendinopathy include pain and stiffness in the tendon during the morning or while exercising.
Diagnosis of Achilles tendinopathy is usually clinical after an examination but your physician may occasionally order imaging such as ultrasound or x-rays. Treatment is usually conservative, not requiring medical intervention.
Lateral Ankle Sprains
Lateral ankle sprains are very common injuries but can be disabling. The term “sprain” refers to damage to a ligament. In ankle sprains, the most commonly injured ligaments are the 3 lateral ligaments (outside) of the ankle. These are the anterior talofibular ligament (ATFL), calcaneofibular ligament (CFL) and posterior talofibular ligament (PTFL). There are 3 grades to sprains; a grade 1 sprain results from stretching of the ligament and microscopic tears, a grade 2 sprain results from a partial tear of the ligament, a grade 3 sprain results from a complete tear of the ligament and can result in joint instability.
Ankle sprains usually result from a rolling type (inversion) injury of the foot, such as planting the foot wrong or falling on it. Symptoms of an ankle sprain can include swelling, bruising, tenderness to touch or instability of the ankle.
Diagnosis of an ankle sprain is usually clinical after an examination. As ankle sprains are so common there has been a lot of research to help your doctor decide whether or not a fracture may be present and whether to send for x-rays. Almost all ankle sprains are treated without surgery.
Ankle Pain Treatments
Ankle Tendinopathy:
Some non-medical treatment options include:
- Exercises to help maintain range of motion and strengthen muscles around affected joints
- Rest
- Ice/Heat
- Orthotics
Some medical treatment options include:
- Pain medications, including Tylenol/Acetaminophen
- Non-steroidal anti-inflammatory medications, including Advil/Ibuprofen and Aleve/Naproxen, and topical formulations (Diclofenac, Voltaren)
- Nitropatch
- Shockwave therapy
Lateral Ankle Sprains:
Some non-medical treatment options include (adapted from Vuurberg et al 2018 Systematic Review):
- Exercises that focus on neuromuscular and proprioceptive exercises to help maintain range of motion and strengthen muscles around affected joints are associated with quicker time to recovery and enhanced outcomes. It is unclear whether this should be supervised or not.
- Immobilisation: If there is significant pain and edema, crutches or an air cast boot can be used short term until patients are able to support weight on their ankle. Studies are suggesting that immobilization should not exceed 10 days.
- Ice can help with pain, swelling, and function if used in combination with exercise therapy
- Functional Support through ankle braces or tape for 4-6 weeks can be very effective. Ideally, a more rigid brace is preferred over elastic bandages or tape.
- Manual therapy/joint mobilisations: Therapists can help with the acute joint pain and decreased range of motion through manual therapy when done in conjunction with other treatments, such as exercise.
- Other therapies: Studies have not found a treatment effect on pain, swelling, function, and return to sports with ultrasound therapy, laser therapy, electrotherapy, and shortwave therapy. Studies on acupuncture are inconclusive at this time.
Some medical treatment options include:
- Pain medications, including Tylenol/Acetaminophen
- Non-steroidal anti-inflammatory medications, including Advil/Ibuprofen and Aleve/Naproxen, and topical formulations (Diclofenac, Voltaren) to help with the acute pain and swelling
- Surgery: If patients have chronic instability after multiple sprains and have not responded to a comprehensive exercise based program, surgery can be considered. Please talk to your physician as this is beyond the scope of this website.
Achilles Tendinopathy Stretches:
| Name | Repetitions/Sets | Description (Basic) | Progression | Modified |
| Heel cord stretch | 3-5 repetitions of 10-30 second holds for each leg. Stretches should be performed 4-6x/week. | Stand facing a wall with your unaffected leg forward with a slight bend at the knee and your affected leg back. Keep both heels flat on the floor and press your hips forward towards the wall and hold. Do the stretch with your back leg straight and with it bent. Do not arch your back. Repeat the stretch for the other leg. | ||
| Towel stretch | 3-5 repetitions of 10-30 second holds for each leg. Stretches should be performed 4-6x/week. | Sit on the floor with both legs in front of you. Loop a towel around the ball of your foot and hold the ends of the towel in your hands. Keep your leg straight and pull the towel towards you. Repeat the stretch for the other leg. |
Achilles Tendinopathy Exercises:
- Ensure proper stretching before attempting exercises.
- Ankle should be mostly pain free prior to attempting.
| Name | Repetitions/Sets | Description (Basic) | Progression | Modified |
| Calf raises | 2-3 sets of 10 repetitions on each leg. Exercises should be performed 3 times per day if possible. | Beginning with both feet flat on ground and weight evenly distributed on both feet. Slowly raise heels off of ground until on tip-toes and then slowly lower heels until back on ground. Once you are doing this pain-free you can proceed to go up to tip-toes rapidly but still make sure to lower heels slowly.
Do this exercise with knee straight and with knees bent to target different muscles.
You may want a chair or table to grab onto to help keep you stable.
Be sure that your ankles are straight throughout the range of motion and that you aren’t bowing to one side. |
Once you are doing the exercise on flat ground painlessly you can progress to doing the exercise on a stair or sturdy box to let your heel hang over the edge and have greater range of motion.
Once you are tolerating the over-hang well using both feet you can begin using one foot.
When you are able to do 30 one-legged calf raises in a row pain free you are ready to return to other activities such as running/jogging. |
If you aren’t yet able to do the exercise completely pain-free you can distribute your weight so that more of your weight is being raised with your healthy ankle. |
Ankle Sprain Stretches
| Name | Repetitions/Sets | Description (Basic) | Progression | Modified |
| Heel cord stretch | 3-5 repetitions of 10-30 second holds for each leg. Stretches should be performed 4-6x/week. | Stand facing a wall with your unaffected leg forward with a slight bend at the knee and your affected leg back. Keep both heels flat on the floor and press your hips forward towards the wall and hold. Do the stretch with your back leg straight and with it bent. Do not arch your back. Repeat the stretch for the other leg. | ||
| Towel stretch | 3-5 repetitions of 10-30 second holds for each leg. Stretches should be performed 4-6x/week. | Sit on the floor with both legs in front of you. Loop a towel around the ball of your foot and hold the ends of the towel in your hands. Keep your leg straight and pull the towel towards you. Repeat the stretch for the other leg. |
Ankle Sprain Exercises:
- Ensure proper stretching before attempting exercises.
- Ankle should be pain-free before attempting exercises.
| Name | Repetitions/Sets | Description (Basic) | Progression | Modified |
| Proprioception training | It is expected that you won’t be able to hold your balance for minutes at a time. Try to hold your balance for as long as you can on-and-off for 2-5 minutes at least once daily. | Ensure that you have enough space and a clear area. You may want a chair or table to grab onto to help catch your balance.
Begin by standing on your affected ankle on flat ground and with your eyes open. Hold this for as long as possible but know that you aren’t expected to be able to hold your balance for the full 2-5 minutes.
Once you are tolerating the exercise with your eyes open, try doing it with your eyes closed.
|
Once you are doing well on a flat surface with your eyes closed you can consider doing the exercise on an unstable surface by adding a cushion, folded towel or a Bosu ball.
For a more advanced version of the exercise add movement when balancing. Consider doing toe touches or bouncing a ball to force you to reach out.
|
Find the level of difficulty that you are comfortable with. If you cannot balance on flat ground with your eyes open then attempt the “Theraband ankle flexion” exercise. |
| Theraband ankle flexion | 2-4 sets of 8-15 repetitions on each leg. Exercises should be performed 4-6x/week. | Wrap a theraband around the ball of your foot and hold the ends in your hands. Begin by moving your ankle up and down against the theraband in a straight line. Once you can do that in a pain-free manner then add up-and-out and up-and-in movements. | Once you are able to do this easily you can add more resistance or move on to proprioception training. |
