Plantar Fasciitis
Introduction
Plantar Fasciitis is a very common condition causing pain in the heel. One study estimated that approximately 10% of the population will develop plantar fasciitis in their lifetime.
Typical signs and symptoms of plantar fasciitis include pain at the heel, pain with the first step after resting or sleeping, and pain that usually improves as you walk. During early push off phase of walking, the plantar fascia is exposed to higher tension, and this is often the most painful movement. Some risk factors for this condition include increased body mass index (BMI), altered gait patterns that stress the plantar fascia more than normal, sudden increased stress to the plantar fascia (such as going for a significantly longer runs or walks than the body is typically used to).
Anatomy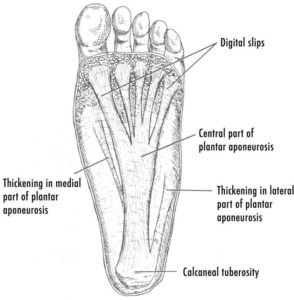
The plantar fascia is a thick fibrous connective tissue at is at the bottom of your foot. This fascia attaches from the medial (inside portion) of the calcaneal tuberosity and divides into branches that attach to each toe. The plantar fascia is filled with densely compacted collagen fibers that are oriented mostly in a longitudinal direction, although some other fibers run transversely and obliquely. Through a windlass mechanism, the plantar fascia helps to support the arch of the foot.
Sometimes people can have a bony outgrown of the calcaneal tuberosity called a plantar calcaneal spur. Current studies suggest that there is a highly variable association between the spur and plantar fasciitis, meaning that this spur is not that cause of plantar fasciitis. The spur typically arises from the intrinsic muscles.
Pathophysiology (What happens in Plantar Fasciitis)
The condition is thought to develop due to excessive strain and overload to the plantar fascia. This causes an inflammatory reaction that leads to the collagen fibers becoming disorganize, which over time disrupts the integrity of the fascia.
Diagnosis
Diagnosis of plantar fasciitis is can be done in the clinical setting with your doctor and does not usually need any further imaging tests. However, your doctor may order some imaging to get more information.
Treatment
This is adapted from the American College of Foot and Ankle Surgeons 2018 Clinical Consensus Statement and American Physical Therapy Association 2014 Guidlines
Some non-medical treatment options include
- Exercises to strengthen and stretch the plantar fascia or Achilles tendon
- Weight loss to reduce stress on the plantar fascia
- Activity restriction
- Ice/Heat
- Biomechanical support – Including Custom orthotics, taping, supportive shoes
- Night splints
Some medical treatment options include
- Pain medications, including Tylenol/Acetaminophen
- Non-steroidal Anti-inflammatory medications, including Advil/Ibuprofen and Aleve/Naproxen, and topical formulations (Voltaren/Diclofenac)
- Shockwave therapy
- Corticosteroid injections
- Other injections such as prolotherapy or platelet rich plasma are often discussed but there are few high quality studies on this type of therapy as of now
- Other therapies such as ultrasound, electrotherapy, low level laser, phonophoresis have conflicting evidence
- Therapies such as trigger point dry needling at not recommended by the American Physical Therapy Association
- Surgical treatment if the other treatments fail (Most people will not need surgical treatment) – including procedures such as plantar fasciotomy. This is beyond the scope of this website.
Exercises
This is a sample program adapted from a program by Caratun et al
Week 1 to 4: Perform 1 set of 10 repetitions using your body weight daily. If unable to do 10, try to do as many as possible.
Week 5 to 12: Perform 1 set of 10 repetitions using increasing weights daily. Fill a backpack with books to increase the weight. The goal is to do 10 repetitions and feel like you are unable to do any more.
Set up
Step 1: Roll up a T-shirt to create a cylinder that you can comfortably wrap your toes around. Adjust the size of the T-shirt accordingly.
Step 2: Place the rolled up T-shirt approximately 5 cm away from the edge of a stair or step and places the toes of the injured foot on it so they wrap around the T-shirt
Step 3: Ensure that the edge of the step is approximately at the halfway point of the foot. Ensure there are rails nearby to hold on to if needed.
Exercise
Perform a heel raise lasting at least 5 seconds going up, pause at the top for 3 seconds, and slowly lower down for 5 seconds.
If possible, perform the heel raise with the other leg in the air.
If this is too hard, heel raises can be done with both feet simultaneously